About Guest Co-Author: Dr Ewan Birney is Associate Director of the EMBL European Bioinformatics Institute and a fellow blogger.
The ACMG recommendations on clinical genomic screening released earlier this year generated quite a storm. Criticisms broadly related to:
- the principle of whether we are ready and able to offer genomic screening to people undergoing exome/genome sequencing (the topic of this post!);
- to whom the recommendations should apply
- whether individuals have a right to refuse genomic screening results; and
- the exact content of the list of genes/variants to be screened.
In the UK, this debate has come into sharp focus following the launch of the NHS 100,000 genome project, where details of data interpretation and data sharing are still rather hazy. The central policy question is clear: in the context of clinical practice, how should we be using genomic data, and with whom, in order to maximise its benefits for patients? (In the context of research, as broad as possible sharing consistent with patient consent is most desirable.) Last month, we published a paper in the BMJ – along with a number of genetic scientists, clinical geneticists and other health specialists – advocating an evidence-based approach that places the emphasis on targeted diagnosis in the short term, and gathering evidence for possible broader uses in future.
(NB. This is not a debate about whether individuals should have access to their genomic information, but a question of what we should expect the clinician’s duty of care to encompass. We both believe that genomic information, along with other aspects of someone’s medical record, should be accessible to the individual.)
Pertinent findings and diagnosis
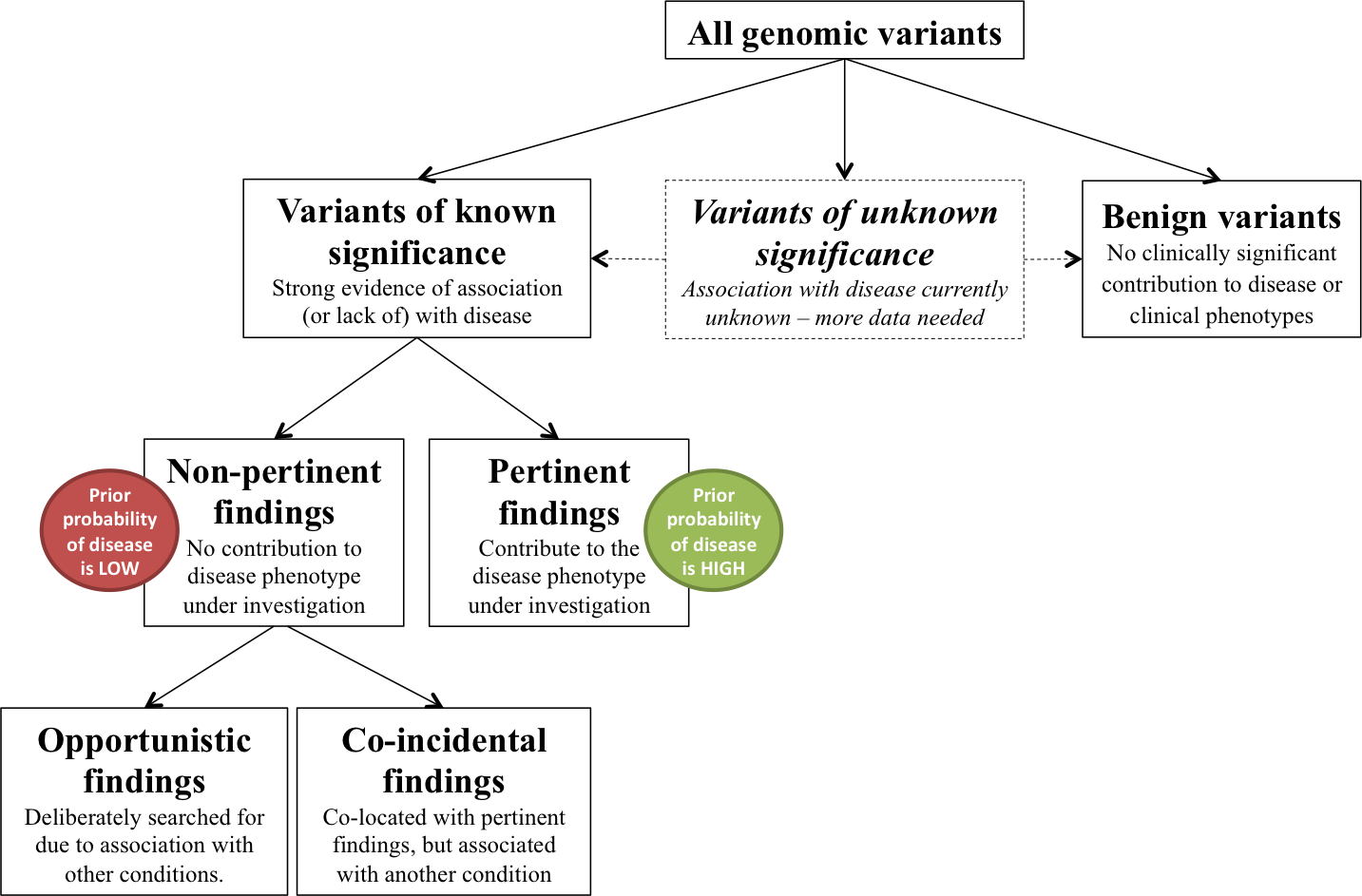
When a genome or exome sequence is determined clinically, there are many variants a clinician could examine. Conceptually, disease variants can be divided into pertinent, i.e. likely to be relevant to the disease phenotype under investigation, and non-pertinent, i.e. everything else. The difference between these two subsets is simply the prior probability of a particular disease in that patient or family (based on symptoms, family history, etc.), which is critical for accurate interpretation of the result.
It is clear that for diagnostic purposes in an affected person, a targeted gene-package approach is underpinned by extensive evidence of the utility of using mutations in specific genes, often stretching back two decades, and sometimes including extensive public health and health economics literature. This targeted gene package might be implemented computationally rather than physically as gene panels, but this mode of using variant data is well established.
Non-pertinent findings and screening
Non-pertinent findings (variously called incidental, accidental, ancillary, secondary, unsolicited, etc.) in an individual at first blush look similar to pertinent findings. After all, the same variant will be pertinent for one patient and non-pertinent to another. However, there is a critical difference: our understanding of the penetrance of variants is nearly always from a series of phenotype-positive scenarios, usually in families, and usually we don’t have evidence about the penetrance in unaffected individuals or families.
Unsurprisingly, where there has been a more extensive exploration of penetrance, the earlier results that often lead to the discovery of the gene were in the most severely affected families. This might be due to other genetic effects, it might be due to environment or it might be due to differential diagnosis. The key point is that a genotype-first diagnosis with no family context is different from an affected family diagnosis, where it is known that a family member has the phenotype in question, and it therefore is a likely genetic cause.
To help clarify the ‘incidental finding’ phrase, we suggest that non-pertinent findings can be further subdivided into two categories: a small number of co-incidental findings, that are accidently and unavoidably uncovered simply by virtue of being either incorrectly categorised or co-located with a pertinent finding, and a potentially large number of opportunistic findings that can be uncovered through a deliberate and directed search strategy.
Co-incidental findings can be likened to other incidental findings that arise throughout medicine, such as a medical imaging, and acting on such findings is a standard part of good clinical practice (an example might be a large CNV that takes out a neurodevelopmental gene as well as a cancer predisposition gene – here, the CNV is the diagnosis, so the co-incidental finding cannot be ignored). In contrast, opportunistic findings are not ‘incidental’ in the true sense of the word, but should instead be considered as an opportunity to offer genomic screening. These opportunistic variants can only be found by deliberately searching for them, and the question is therefore whether we should actively choose to screen individuals’ genomes for a plethora of diseases and traits.
Experience (and human nature) tells us that it is easy to overstate the benefits of screening whilst underestimating the harms from inappropriate treatment and worry. Another key aspect of screening is that it is only beneficial when there is a sensible intervention (and notice that for non-pertinent findings, the benefit of ending the ‘diagnostic odyssey’ is not present; indeed, quite the contrary). As we stated in the paper: “each variant-disease relation must be evaluated separately in light of the evidence associating them and the availability, invasiveness, and cost of confirmatory testing and treatment.” For example, well-characterised and easily treatable diseases for which the benefits of cascade screening of relatives have already been established could be initial candidates for opportunistic genomic screening. Familial hyperlipidemia and hypertrophic cardiomyopathy are two cases where there is routine use of targeted genetic testing and experience of cascading genetic information across families that improves health outcomes – but every gene/disease/intervention would need to be assessed carefully first, just like any other non-genetic screening procedure.
The way forward
We are positive about the use of genomic information for diagnosis, particularly in rare diseases, and for research into the underlying causes of genetic disease. We are also cautiously optimistic about using genetic information for opportunistic screening in future, if the benefits outweigh the harms and a good case can be made in line with best practice for screening procedures. For example, conditions where cascade testing in affected families has proven utility and cost effectiveness – such as hyperlipidemias and hypertrophic cardiomyopathy – could be good initial candidates (if genetic screening in affected families is not beneficial, it almost certainly won’t be in the population).
However there is not, currently, the evidence base to justify opportunistic genomic screening, and collecting this evidence should be a pre-requisite for any considered use of genomic information in opportunistic screening. A key component of this will be determining the population-ascertained penetrance of variants. For instance, if you only have genotype information on a specific class of variants, such as a loss of function allele, how often does this convert to an actionable phenotype? This information could be gathered piecemeal for each set of genes and disorders, but the number of well established disease genes – such as hyperlipidemias, inherited cardiac conditions (which includes the monster gene, titin) and germ-line cancer predispositions – means that a substantial proportion of the exome is already part of diagnostic panel, arguing for a more systematic, genome-wide approach in the context of a cohort with good follow up and global data sharing. This information could then provide a starting point for a rigorous proposal for opportunistic screening guidelines.
This article was cross-posted on the Wellcome Trust Sanger Institute blog.








 RSS
RSS Twitter
Twitter
Excellent article – we’ve been thinking about this in great detail in the context of the (non-clinical) 1958 Birth Cohort – but what consent would the “cohort with good follow up and global data sharing” require? Effectively these people would be volunteering for opportunistic screening, just to get the stats in.
Would you sign up to something that said:
Now, we intend to test all the genetic variants that people have thought contribute to disease, in the hope that you won’t have the “bad” versions of most of them. If you do, we won’t know what it means, but we’ll be watching and waiting …
Actually, there are people who would (and do, with George Church’s assistance) agree to the above, but it seems the NHS 100,000 study you reference assumes clinical and genomic data can be shared with impunity because it will be “anonymised”. While this claim lacks credibility, and may have been made as it means the data escapes EU Data Protection legislation and becomes a portable and saleable asset, it also ignores the legitimate claims of patient feedback within that group.